From the Editor: Happy Mother’s Day! I’m so honored to share #PrettyPerfectWoman Wendelyn’s (of Suits, Scandal and the Good Wife) story with you. One thing I have learned over the last few years, is that life comes at you HARD and with no warning. One second everything is going great and then it isn’t. Wendy’s story is one of perseverance and indescribable love, and I am so grateful she dug deep to share her darkest yet brightest parts with us. Enjoy.
**** Wendy’s Preemie Birth Story****
Chijioke (CJ) and I met, dated, got engaged and married within a year. February, March, September, February. We spent every hour we weren’t at work, and some work hours , together. I’ve read that when you meet the person you are supposed to spend the rest of your life with, you want the rest of your life to begin immediately! That’s us. In our typical fashion, we got pregnant a month after our honeymoon. Our wedding was on 25 February, 2017 and our baby’s Expected Delivery Date was 26 December, 2017.

My pregnancy was, as doctors say, “Unremarkable”. Besides the extreme tiredness and teenage-male hunger levels, I had little sickness. On October 09, 2017 I left my office for a routine antenatal class at the hospital. The hospital was so busy that I decided to return to work and join the next antenatal class on the following Monday. I figured that as I felt fine and my child was active, the antenatal could wait a week.
I rang CJ to tell him I’d be playing truant from the day’s antenatal class. My husband, who was MORE pregnant than I was, absolutely refused and insisted I wait to be seen. The travails of submission. I sat for the antenatal class uninvolved and irritated until the nurse taking my vital signs (required for each antenatal class), said, “You have to see the doctor.”
Oh no ma’am, that is NOT how this works. I wanted to tell her. No, I come for antenatal class to fulfil all righteousness. You crack jokes about my blood pressure being too good and my living stress-free despite a hellish Nigeria, I submit my clear urine test and go home.
We laughed but I could see her smile stopped around her cheeks, her eyes said different as she ushered me to the bed to measure my baby’s size and check the heartbeat. When she called a second nurse to verify her findings, I began to worry.
Nurse 1: “He’s measuring 27 weeks but he should be getting to 29…”
Nurse 2: “He measured 25 weeks when he should have been 27, it might be a pattern…”
Wendy: “Is there a problem?”
Both nurses: “You need to see the doctor!”
They explained that my blood pressure was very high, the urine test indicated a high protein presence and the baby appeared smaller than expected. Causes for concern individually and anxiety cumulatively. One disadvantage of having a largely unremarkable pregnancy is you might take things for granted; I rang my husband just to keep him updated but assured him it was probably nothing major. I walked to the doctors’ room concerned but certain that the nurses’ worries would be satisfactorily dismissed.

The doctor was a reticent, serious, petite woman and the room remained stonily silent as she went about the tasks of conducting an ultrasound and re-checking my blood pressure. Then she checked it again. And again. She began typing furiously on her keyboard, each click increasing my anxiety, until she stopped, grabbed her phone and demanded, “Prepare a bed in the ICU…and bring a wheelchair to my office, now!”
I sat there feeling rather sorry for the poor fellow about to be wheeled into the ICU and mildly upset that the doctor was handling another patient’s matter while I was sat in her office. I consoled myself with the fact that it must be very serious and urgent for her to be doing this in front of a patient.
Then she dropped the phone.
“I’m admitting you into the ICU now for close monitoring. Your blood pressure is very high and the water around the baby is lower than normal.”
Looooooool, WHAT?!
Sorry.
“What? Why?” I croaked, my throat suddenly constricted. I quickly text my husband to come, because I did not understand what the doctor was explaining in her hushed, hurried tones.
My husband rushed to the hospital and we listened to the doctor explain that Preeclampsia was suspected. My husband mentioned our intention to have the baby out of Nigeria, we were scheduled to travel in two weeks, we wanted the best healthcare for child and mother. The doctor stared incredulously at us and intoned, “We most likely have to bring the baby out tomorrow.”
I was lying in a bed away from the doctor and my husband, so I was not sure I’d heard the doctor correctly. Chijioke came towards me and I will never forget the look of suppressed panic and terror in his eyes, his voice was hollow when he asked, “Did you hear her? She says they might have to take the baby out.” I was certain the doctor had misdiagnosed the severity of the situation, my child was still active and I felt fine, so I refused to accept her words and eventually went to sleep.
I woke up the next morning to find the Matron, gynecologist and Chief Medical Officer gathered around my bed attempting to explain that my symptoms indicated I had Preeclampsia which had to be managed to prevent Eclampsia.
Preeclampsia is when your blood pressure becomes high enough to damage your arteries and other blood vessels, and organs begin to malfunction. Damage to your arteries may restrict blood flow. It can produce swelling in the blood vessels in your brain and to your growing baby. If this swelling interferes with your brain’s ability to function, seizures may occur (Eclampsia). HEALTHLINE.
Delivering the baby is the only way to cure Preeclampsia. My baby was 29 weeks. We had 11 weeks left before my scheduled delivery date.
“Preeclampsia usually only happens in first pregnancies. There is nothing to indicate that you will have the same issue in your next pregnancy.”
“The condition deteriorates quickly and there’s no telling what might happen to you or the baby if we don’t take it out now.”
“You’re my patient, I am most concerned about saving your life.”
“You will have other children…”
Now, that is what made me snap out and focus in on the conversation! I only asked one question.
“What are my baby’s chances of survival right now?” Twenty-nine weeks of a forty-week journey, what are the chances of survival in a moderately-equipped hospital in Port Harcourt, southern Nigeria?
“50-50. We cannot guarantee anything.”
I was angry and raged at them wondering why they would consider the drastic measure of pulling out my baby with stakes so low. What a gamble! Leave the baby in me, I insisted, as my baby kicked merrily in my womb, unaware of the plot for imminent evacuation.
They cajoled, they reasoned, they forced, they complained.
I insisted.
I refused treatment and the hospital eventually requested I sign a form absolving them of medical responsibility for my death or the baby’s. I don’t think that hospital will forget us in a hurry! Lol. My parents and in-laws, particularly my mother-in-law who is a surgeon, descended on the hospital management with the force of a small hurricane. There is nothing like a strong support system. They used every contact they had and we got several opinions on the best course of action. I spoke to my good friends and gynecologists Tomi Oke and Ojone Idiakhoa and took photos of every result I got. These two UK-based doctors shared the photos and daily reports with their supervisors and really encouraged me. It was important to get the opinions of my close childhood friends who knew me, understood my family, and brought the advantage of a different healthcare system. The medical opinion was the same from every angle, “29 weeks is very early. Wait it out for as long as possible…until something changes.”
No matter how I tried, the blood pressure and proteinuria seemed to rise in those four days in the ICU. There were moments of optimism when both would appear to drop, but they would suddenly spike again without provocation. I constantly oscillated between calm assurance that all would be well and uncontrollable panic for my baby’s life and mine. It was horrid. I could not stop crying. I was afraid. I kept praying, trusting God to do something heroic, miraculous, to save me from the seemingly unending nightmare. I could not understand. Why me? Was I not careful enough in my pregnancy? Could I have prevented this? Was this some delayed punishment for something I had done earlier in life? Did we do something as a couple to deserve this?
Every day the doctors reminded me that Preeclampsia deteriorates fast, so every moment wasted could be fatal to mother and child. I was unmoved. To me, every additional day in the womb strengthened my child and I would do anything to give him another day, another chance. Regardless of my stance, the doctors gave injections to prepare the baby’s lungs in case of an emergency delivery and moved me to the Maternity ward.
I remember being wheeled into the ward and tearing up at the sight of the baby cots placed next to each bed. “Will I ever get to lay my child in one of these?” I wondered. The fact that I was in the Maternity ward not the ICU gave me some relief. Finally, everything seemed under control.
Then Friday happened.
In the Maternity ward, a cardiotocography test is done several times a day to check for any irregularities in the baby’s heartbeat. I was hooked up to the machine as my husband and I sat enjoying the last visiting hour that Friday evening. Chijioke took photos of the results for Tomi and Ojone who had told us the heart rate should be within the 160-180 range, so we were surprised to see it drop to 34, 40…then slowly rise. We noticed this dip twice. The first time it happened, my husband spoke to the nurses who assured us that things were fine. At the second dip, he did not have to speak to anyone. The formerly quiet ward was a sudden hive of activity as all the nurses dove into action. We heard the head nurse call the doctor then repeat the gynecologists’ words loudly, “Prepare for surgery”.
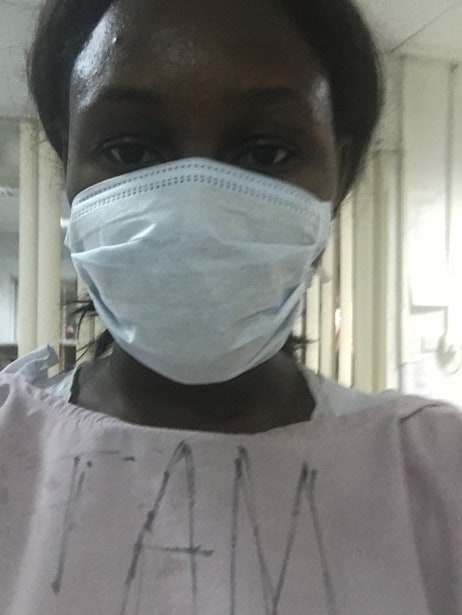
In two minutes (MAX!), I was naked, shaved, robed, and ready to be wheeled into the theatre. My fear could not be quantified. Rebellious till the end, I fought every step of the way with cries of, “I am not taking my baby out, I feel fine”. Lol, try doing this as someone secures an oxygen mask over your nose, gives you injections, inserts a cannula in your hand and a catheter in your privates! A preview of hell.

The gynecologist appeared at my bedside and asked the activity to stop momentarily, then said in her quiet but resolute way, “Wendy, give your baby a chance.”
I went limp.
They wheeled me into the theatre and preparations began. I needed an emergency Caesarean Section because a vaginal birth would put too much stress on the baby at that point. Later, I realized my husband had called my friend Dr. Ojone to ask her opinion on the surgery before they wheeled me into the theatre. She said if things had reached this critical point, there was nothing to be done but remove the baby. CJ got some peace from that assurance that this was the best cause of action. I didn’t. I didn’t know if this was the right thing to do, but I felt that it was the only choice we had considering the circumstances. Still I was doubtful, torn, so afraid that my entire body was wracked with tremors. I overheard the gynecologist ask the anesthesiologist, “She is trembling badly, is she reacting to the anesthesia?” He whispered, “No. I think she is just terrified.”
The entire time I kept expecting God to intervene and stop things. In fact, in the theatre, there was a long break before the surgery as the lab assistants searched for something to dissolve my acrylic nails (see the Baby Shower photo above for the nails) before the operation. I thought, “Aha! This must be God about to rescue me from all this! A true 11th hour miracle to make my testimony unique!” Yeah, I was wheeled into surgery y’all! No close shave, no last save. I felt defeated. I kept thinking “WHERE ARE YOU GOD? WHY ARE YOU DOING THIS? HOW CAN YOU LEAVE ME ALONE, NOW?” My thoughts growing increasingly incredulous with each question. And then the first cut came and stole my breath. I do not know how anyone can look down on a Caesarean Section as taking the easy way out. The terrifying, strange, violating feeling of having hands roam around your insides, shifting and tugging delicate organs as they race against time, is better imagined. A 45-minute surgery took almost 4 hours as my child was settled around my diaphragm, forcing the doctor to request another doctor bear down on my chest as a suction machine was used to gently pull out the baby. The operation seemed unending and I was scared throughout the process: Scared of dying, losing the baby or just some further complication as the blood pressure continued to spike. I could hear myself chanting, “Please God, help me please God…” Finally I heard Kaito’s shrill, enraged cry.
“You have a son!”
“1.08kg!” they cried as they showed me my baby boy for a second before sprinting to the Nursery Intensive Care Unit (NICU) with a mobile incubator. I was relieved. At least he was over 1kilogram! The doctors had expected him to weigh less. I saw my blood pressure slowly drop as soon as the baby was removed. I was relieved, but as the doctors began sewing me closed, I began to feel excruciating pain with every tug of the needle. I screamed, to the surprise of the doctors, and they initially suggested it was pressure not pain I was feeling. I was prepared to agree, certain that fear was playing tricks on my mind, until the needle pierced the flesh of my uterus again. No. No! PAIN.
They put me to sleep immediately.
I woke up the next morning from what felt like a kick in my stomach and smiled in relief. What a nightmare! Then reality dawned, it HAD happened. I was not pregnant anymore.
Terror seized me as I limped to see my baby in the NICU for the first time. Did he survive? Were there complications? Do I have the strength to face what I might see? I wasn’t sure I could handle it until a nurse gently reminded me that my baby needed my encouragement to survive.
I walked in and saw Kaitochukwu for the first time.

Chijioke came and I learnt that my husband, parents and in-laws had camped outside the theatre panicked when the 45-minute procedure extended for over 4 hours. My husband was broken, afraid of losing his wife and child at once. He had been my rock through five of the hardest days of my life. He was the one that told me to take the baby out if it would save my life because, “If only one preterm baby can survive, anywhere in the world, it will be our child”. Confidence. He always seems so confident but the reality of my surgery had broken him and I could see it. That day we sat, quiet but happy. We made it. All three of us. 8 months into our marriage, we’d won the greatest battle.
We did not know the war had just begun.
The first time I saw my son Kaito, he looked so little and helpless. How could I have been afraid to see him when he clearly needs me? I asked myself as I stared at his tiny chest rising and falling rapidly. Oxygen mask fitted over his head and covering his nose, a monitor strapped to his leg measuring oxygen circulation in his blood and heart rate, intravenous tube giving him extra protection with antibiotics and fortified nutrients through his belly button, a feeding tube directly into his stomach…and those boxing gloves because this little hero is pulling everything off as soon as you let him! My heart just broke. This is not how you dream of meeting your child for the first time.

There was no time for a pity party though, CJ and I understood our role. We have a child and must do everything to secure his survival. We researched, questioned, sought advice from pediatricians around the world especially my friend Dr. Ada Adejoro (@ask_dr_ada), to make sure we understood everything we could about his care, the expectations and ways to help. The most practical way to help, besides praying constantly, was to provide breastmilk for nourishment. After the surgery, my blood pressure had spiked again and I was informed that it would take 6 weeks, at least, to determine whether I would now be hypertensive for life, or the high blood pressure was the result of my pregnancy. I had to remain in hospital supervised. Possibly due to the stress and shock of these things, my milk supply was low. The nurses were such an amazing support. They would sit and squeeze my body at odd hours until we had enough to feed the baby. They would try to be gentle because it was clear I was in pain but I would always encourage them to ignore the pain and focus on the purpose: breastmilk aka Liquid Gold.
My parents and in-laws came daily to pray and just cheer us up, everyone was confident that the worst was over, after all Kaito had cried so loudly at birth he had to be fine, right?
Buoyed by the confidence of our families, CJ and I spoke to the pediatrician on Sunday. The pediatrician was truly a gift from God. She was a soft-spoken woman with a strong air of competence and empathetic ways. CJ and I liked her immediately, certain that things were going to be fine now. Then sShe hit us with reality, telling us to take each day as it comes and not get our hopes up. Kaito was the smallest child they had managed at the hospital even though he was not the youngest. She explained that preterm infants tend to do well initially but as the immunity from the womb wears off, they are left to face the complications of the world with whatever capacity they have developed in the womb. In other words, no one can tell how well a preterm baby will do…until they DO. It was hard to hear her say the next 7-14 days were critical as many preterm babies tend to lose weight, fall sick from infections and many do not make it out of that period alive.
“I just wish we could see ourselves this time next Sunday” we both muttered as we squeezed into my tiny hospital cot like two puppies finding shelter from the rain. It hadn’t rained on our eight-month marriage, it had flooded. There is no worse feeling than going to bed everyday with the haunting possibility of not finding your child alive when you wake up the next day. Sleep is difficult when you know that a complication can occur in the middle of the night. The baby was in the NICU, I was in the Maternity ward, CJ was at home. Separated, solitary and sad. We were told we had at least 9 weeks to stay in hospital, as he would only be released home around his due date, IF he made it. Those wedding vows suddenly became very real.

We learnt the strength of joint sorrow on days we lived in fear of the onset of infections and setback in Kaito’s recovery. We knew joy when he hit milestones the doctors were unsure he could, indescribable love at those times he seemed to turn his head and stare at us with a simple curiosity. We understood friendship, partnership, when no one else can understand the strange space of receiving congratulations for a child you’ve never held. We mined our souls and found illogical patience and a deeper love and respect for each other as the days trickled by in small increases in feeding and weight measurements. On the days it seemed too long and too much to bear, I would remind my husband, “Don’t worry Obi’m, next year has to sha come.” When it’s so hard to see beyond today, I would remind him that tomorrow would still happen no matter what today brought.
I think my pain was easier to see, to process or understand. One day my husband told me that everyone can comfort me easily because they can physically see the pain I am living through. It’s easy to forget that he is also dealing with the same fears and sorrow. And it is true, men often get left out in the history of our fights for children whether its infertility or other pregnancy-related complication. It seems like a woman’s fight. But, it is not. I had a great circle of friends to hold my hand and cry with me, in fact some days I would call one of my best friends, Anne and WAIL for ten minutes straight, then drop the phone. My mum, sisters, mother-in-law and sister-in-law constantly checked on me. We were a unit. And, I journaled to help me process…but many men don’t have a system for processing grief and fear. Worse, what nobody says about grief is that it is selfish. The days our child was in the NICU found my husband and I sometimes leaning on each other, heavily, chokingly, for support. At other times, we were barely surviving as a unit, each swallowed up in an individual, turbulent sea of sorrow, anxiety and fear. We were both trying to, barely, keep ourselves afloat. At that point, all your energy is focused on keeping yourself together, preventing yourself from a total breakdown that you have neither the space nor strength to support anyone else. On other days, you lean on each other with a desperation that only the other person, the other parent, can understand. Nothing unites two people deeper than the joint fear of losing your only child.
We learnt that lesson in the sleepless nights where panicked doctors would rush into the NICU (connected to the Maternity ward through an adjoining door) and I would immediately wake up and text CJ to stay alert and pray, giving him updates constantly. I eavesdropped on nurses shamelessly, consistently. My husband arrived at the hospital, randomly, always terrified if he rang my mobile twice and I didn’t answer. CJ, my extrovert of a husband, is lovable and favoured, he makes friends everywhere he goes. Soon the nurses began to monitor me to make sure I carried my phone everywhere to answer his calls on the first ring. “Don’t scare your husband!” Lol so who should I scare instead?!
I prayed. I prayed constantly. Deeply. Desperately. I have been Christian long enough to know that God’s will may not always be what I consider a positive response to my request. I knew it could also be within the will of God to lose a child and use that loss as a platform to engage others, to grow a deeper faith. Like Abraham. I understood and all I prayed for constantly was for God to show me mercy and preserve my child’s life. I promised that whether He gave us Kaito or not, we would consecrate ourselves to Him. We created an educational fund in honour of our child to sponsor the best-performing child of the nurses in a tertiary institution annually. A commitment we were dedicated to keeping either in memory of our son or for him to inherit and become a part of.
Eventually, things began to look up. The wires were slowly disconnected from Kaito. First the oxygen tube as his lungs matured enough to breathe on his own, then the antibiotics, then the feeding tube, then the monitors. He was healthy, strong, and doing very well, only remaining in the incubator to reach the hospital’s target weight before release. We were incredibly blessed, Kaito did not suffer any complications from the prematurity besides being small at birth.
Soon we began to have our own unique firsts as parents.



The hospital operated a minimal contact policy for preterm babies and non-medical personnel until the infant was out of the incubator. My blood pressure was back to normal after about 6 weeks and I was in hospital mainly to be with my baby. However due to the hospital’s policy, I was still unable to do more than look at the baby. At night I would cry into my pillow surrounded by new mothers nursing and cuddling their newborns. I asked to be discharged. I would come from home with breastmilk 4-5 times a day and visit the NICU at the same rate as I did when I was a patient in the hospital. Some of the other mothers in the ward overheard my discussion with the doctors and were not pleased. LOL. With side barbs and sarcasm I was soon scolded and informed that it was irresponsible to put myself before others, as a mother. Fortunately, I could not care less if I tried because I believe this legal maxim to be true: “Nemo Dat Quod Non Habet”. “You Cannot Give What You do not Have”. Often women martyr themselves at the altar of others forgetting that to truly serve and love, you must be whole. Wholeness for me was not in a ward of resentful women and fretful newborns. It was at home preparing a nursery in faith of my new born’s arrival, with the support of a husband who is my dearest confidante and closest friend. That experience taught me to be kinder, everyone is fighting a battle bigger than you know.
Finally, Kaito reached the target weight and we began to complete our immunizations and prepare to leave the hospital that had been part of our lives since I walked in for antenatal classes on that fateful Monday.

After 65 days in intensive care with doctor and nurses watching him every minute of each day, Kaito got a chance to sleep in his mother’s arms, in his father’s house. We were frightened; still newlyweds and even newer parents, and I wanted to beg the entire medical team to retire to the house with us. I was worried I would make mistakes and reverse all the hard work that had been done by the most amazing team of doctors and nurses I have ever met. Chijioke, in true CJ style, was confident (nothing shakes this man y’all!) we would be fine and Kaito would thrive. As always, his confidence buoyed me.
Kaito is 6 months now, strong, healthy and active. He loves bath time, thinks every touch is a call to play, laughs loudly and is incredibly observant. With the support of our amazing (AMAZING) parents, the best siblings and incredible friends, Chijioke, Kaito and I lived through hell…and are stronger for it. If you’re going through a NICU journey all I will say is, “Next year will sha come.” Meaning, it will not always be like this. There are much better days ahead than any we leave behind.
Trust God.




(Kaitochukwu: Let Us (All) Praise God)
About the Author: Wendelyn is a wife, mother, lawyer and feminist who believes a woman reserves the right to determine who she is…and in what order ;). She works in the corporate social responsibility space and runs the blog www.